Abstract
Introduction
T-lymphoblastic leukemia/lymphomas (T-ALL/LBL) are immature T-lymphoid neoplasms localizing in the bone marrow, mediastinum, central nervous system, and lymphoid organs. T-ALL/LBL accounts for 10 - 15% of pediatric and 25% of adult acute lymphoblastic leukemia (ALL) cases. Historically, the outcome of adult patients with newly diagnosed T-ALL/LBL) has been poor. Various studies reported low complete remission (CR) rates and short median overall survival (OS) ranging from 11 to 17 months. Here we present real-world data on outcomes and characteristics of an ethnically diverse adult population with T-ALL/LBL treated in a large academic center.
Methods
A retrospective chart review was performed of all patients with pathologic diagnosis of T-ALL/LBL at Los Angeles County + University of Southern California Medical Center and Norris Comprehensive Cancer Center. We identified thirty-one patients between January 1st, 2011 and January 1st, 2020. Demographic, clinical, and pathologic data were extracted from the medical record. Data analysis software SAS (9.4) was used to assess overall survival (OS).
Results
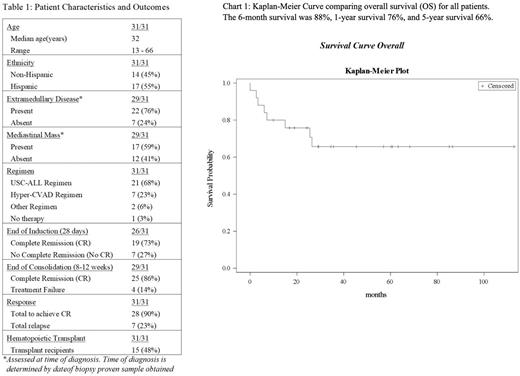
In our cohort, 61% were male and 55% were Hispanic. Median age at diagnosis was 32 (13 - 66) years (table 1). Median white blood cell count (WBC) at presentation was 81,000 (1,800 - 526,000) 109/L. Median peripheral blast percentage at presentation was 35% (0% - 91%), with 23% (7/31) having no peripheral blasts. Median bone marrow blast percentage at diagnosis was 68% (0% - 97%), with 30% (9/30) having <20% blasts. Extramedullary disease was present in 76% (22/29) at diagnosis, with 59% (17/29) presenting with bulky mediastinal disease and 3% (1/31) with central-nervous-system (CNS) disease. Early T-cell precursor phenotype was noted in 16% (5/31) and complex cytogenetics in 18% (5/28).
The most common regimen was the pediatric-inspired USC-ALL regimen (based on CCG-1882), 68% (21/31), and the next most common was hyper-CVAD regimen, 23% (7/31). Two patients received alternative regimens and one patient did not receive therapy. 90% achieved CR using the definition of bone marrow blasts <5% and resolution of extramedullary disease. Seven patients (23%) relapsed after achieving CR. Median follow-up for our cohort was 26.5 months, with 71% followed at 1-year, and 58% followed at 2-years. At the time of the study, 17 patients (55%) were known to be alive, and 8 patients (26%) were deceased. Hematopoietic stem cell transplantation (HSCT) was performed in 48% (15/31). The OS was 76% at 1-year and 66% at 5-years.
Conclusions
According to MD Anderson group, a CR rate of 91% and 5-year OS rate of 67% were reported with hyper-CVAD in T-ALL/LBL patients. Similar results were reported with Berlin-Frankfurt-Munster and the UK ALL XII/ECOG 2993 protocols. Our data reflects a comparable outcome in this predominantly Hispanic adult T-ALL population. Increased utilization of allogeneic HSCT might have been attributed to improvement in survival. Currently, very limited data is available exploring diverse racial and ethnic groups in this disease and we hope our cohort is an addition to the process of better understanding the social and phenotypic differences in T-ALL characteristics and outcomes.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal